5 MAJOR CAUSES OF IVF FAILURE.

Embryo transfer is a critical step in the In Vitro Fertilization (IVF) process. Even when good-quality embryos are used, some transfers still fail. Below are five major causes of such failures, along with explanations and solutions. Uterine Issues The uterus (womb) must be in optimal condition for an embryo to successfully implant. Several problems within the uterus can prevent this: Polyps: These are small growths inside the uterine lining that can interfere with implantation. Adhesions (Asherman’s Syndrome): Scar tissue inside the uterus, usually from past surgeries or infections, can block implantation. Fibroids: These are non-cancerous growths. If they are within or near the uterine cavity, they can distort it and reduce success rates. Ulterine cavity abnormalities A uterus that is not “free” or open (e.g., narrow cavity) cannot support embryo implantation properly. Doctors often recommend a hysteroscopy before starting IVF. This procedure allows them to see inside the uterus and remove any obstacles (polyps, fibroids, scar tissue, etc.) that may hinder implantation. Hydrosalpinx This refers to a condition where the fallopian tubes are swollen and filled with fluid, often due to previous infections (like pelvic inflammatory disease). The fimbriae (finger-like ends of the fallopian tubes) become blocked. The fluid from the tubes can leak into the uterus and harm the embryos, making implantation unlikely. Hydrosalpinx must be treated before IVF begins. Often, the fallopian tubes are removed (salpingectomy) or blocked off to prevent the toxic fluid from reaching the uterus. Inadequate Fertility Treatment (Hormonal Imbalance) Hormones must be in the right balance for IVF to work. Key hormones include: LH (Luteinizing Hormone) FSH (Follicle-Stimulating Hormone) AMH (Anti-Müllerian Hormone) – an indicator of ovarian reserve If any of these are out of range, the body may not respond well to fertility medication, resulting in poor egg quality or uterine lining problems. Get your hormone levels tested before treatment. If there’s an imbalance, your doctor may recommend hormone therapy or other medications for 1-2 months to stabilize your system before IVF. Poor Embryo Quality Even if everything is perfect in the uterus, if the embryo itself is not healthy, implantation will likely fail. Embryos are graded (e.g., Grade A, B) based on how they look under a microscope. The developmental stage also matters Blastocyst (Day 5 embryo) is usually preferred over earlier stages (e.g., morula). Poorly graded embryos have lower chances of implantation and pregnancy. Ask about the quality and grade of the embryo being transferred. Consider genetic testing (PGT-A) if you’ve had repeated failures, to check for chromosomal abnormalities Difficulty During Embryo Transfer Procedure Even if the embryo is good and the uterus is healthy, technical issues during the transfer can cause failure: Cervical stenosis: Narrow or tight cervix that makes it hard to insert the catheter. Uterine angle or position: May make the passage of the catheter difficult. Bloody transfer: If the catheter causes trauma and bleeding during the procedure, blood can be toxic to the embryo. Vaginal stenosis: Narrowing of the vaginal canal, possibly from past procedures or radiation therapy, can complicate the transfer. A sono-hysterogram or mock transfer may be done in advance to check if the cervix is easy to pass. If stenosis is detected, cervical dilatation may be done beforehand. Ensure a skilled clinician is performing the embryo transfer with utmost precision.
ENDOMETRIOSIS
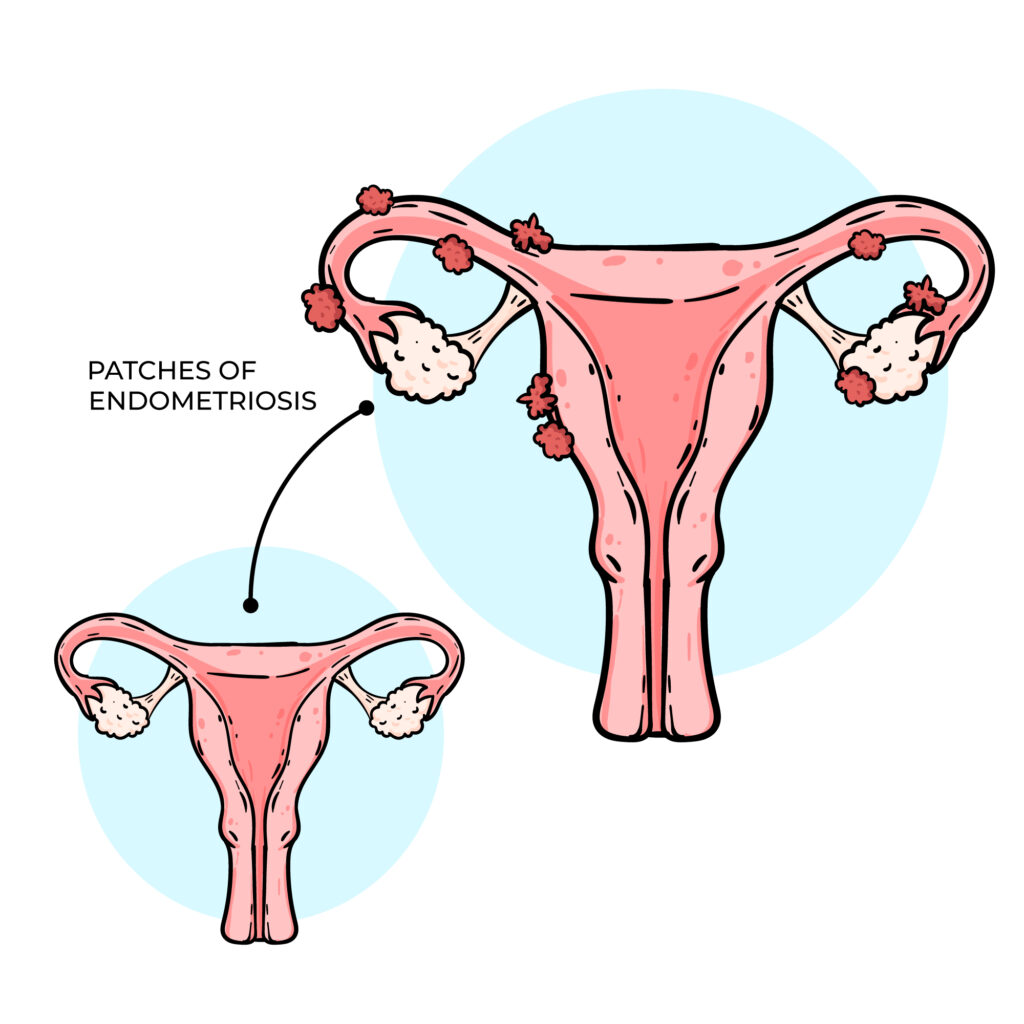
Endometriosis occurs when the tissue that normally lines the uterus and sheds during menstruation grows outside its usual place, often causing painful periods and affecting fertility. This tissue can grow within the womb’s lining and continue to spread as long as menstruation continues. Complete removal is usually not possible, as taking out too much can damage the uterus and affect the ability to carry a pregnancy, In severe cases, surgery may be done to remove some of the tissue, followed by hormone injections that stop menstruation for 3-6 months, allowing remaining tissue to shrink. However, a more effective approach may be to register with an IVF clinic, undergo endometriosis surgery, and then begin IVF treatment while menstruation is suppressed. This gives the body a better chance to conceive while preventing further tissue growth. It’s important to check and balance your AMH levels and hormones before surgery to improve your chances of success.
